Key Takeaways
- The health of your immune system is mostly determined by lifestyle choices and your environment, not your genetics.
- The most effective ways to support your immune system are to exercise regularly, sleep at least 7 to 9 hours per night, manage your stress levels, and limit your alcohol intake.
- Keep reading to learn exactly how to implement each one of these strategies to maximize your immune function and minimize your chances of getting sick!
If you’re like most people, you’ve been paying attention to what’s happening with coronavirus.
Over 300,000 people have taken ill as of this writing and, depending on who you ask, the death rate ranges from 0.3 to 1 to 3% (one of the latest studies pins this number right in the middle at 1.4%).
This makes it slightly more deadly than the flu, and significantly more deadly for those who are over 60 years old.
While it’s easy to blow the situation out of proportion (and the media firestorm isn’t helping), it’s still wise to do everything you can to shore up your immune system in times like these.
You’re probably already taking preventative measures like washing your hands, avoiding large crowds, and so forth, but you’re still exposed to thousands of different germs every day (and possibly, COVID-19). That’s not to mention the thousands of other seasonal diseases that sweep around the world every year like a swarm of locusts.
And if one of these germs manages to sneak past your guard, it’s up to your immune system to knock them out before they make you sick.
That raises the question: can you do anything to boost your immune system?
If so, which methods work and which don’t?
You’ll learn the answers to all of those questions and more in this article.
So, let’s start with discussing what the immune system is and how it works, and then we’ll get to how to strengthen it and how to prevent and quickly overcome illnesses.
How the Immune System Works

The immune system is a network of cells, tissues, and organs that work together to identify, kill, and purge infectious diseases from the body.
While the intricacies of the immune system are endlessly complex, here’s the abridged version:
A virus, bacterium, or other pathogen manages to sneak into the body.
Specialized white blood cells known as B lymphocytes, which you can think of as sentries maintaining watch and ward throughout your body, quickly identify the intruders.
They mount an initial defense by blasting the pathogens with small proteins called antibodies, which serve a few purposes:
- They mark the invading pathogens as persona non grata, kind of like the dye packs used to mark bank robbers, making them easier for your body to identify.
- They make it more difficult for the pathogen to enter healthy cells.
- In the case of bacteria, they neutralize some of the toxins produced by the bacteria.
- And perhaps most importantly, antibodies alert more vicious and effective immune cells to the presence of invaders.
If B lymphocytes are like beat cops, T lymphocytes are like heavily armed SWAT cops bristling with guns, swaddled in body armor, and eager to utterly decimate whatever gets in their way.
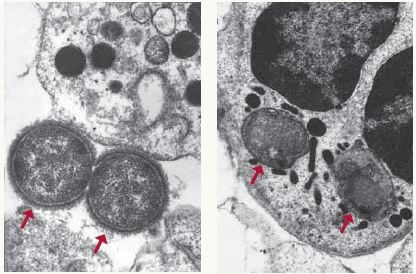
Using the antibodies to identify their enemy, T lymphocytes (also called “T killer cells”) wade into the pathogens, literally shooting them with a substance called perforin, which pierces the cell walls of bacteria or infected cells, causing them to “bleed out” and die. Other immune cells known as natural killer cells operate in much the same way, using a variety of different toxins and enzymes to hack pathogens and infected cells apart and break down the remnants.
Another specialized immune cell known as a phagocyte literally eats viruses and bacteria, swallowing them whole and using various enzymes to break them down. You can see a phagocyte eating two Neisseria gonorrhoeae bacteria (marked by red arrows), the bacteria that causes gonorrhea, in this microscope image:
There are other elements of the immune system, such as the lymph system which filters viruses and bacteria from the body, and the spleen, which serves as a kind of home base for immune cells, but that’s the long and short of it.
There are many factors that determine how well this system works, including diet, sleep and exercise habits, stress levels, germ exposure at a young age, and vaccination history. Luckily for us, research conducted by scientists at the Karolinska Institute shows that our genetics only determine around 25% of our immune system health, with the other 75% being determined by lifestyle choices and our environment.
In other words, most of your immune system health is in your hands. Keep reading to learn how to improve it!
Summary: The immune system is a complex network of cells, tissues, and organs that works to identify, kill, and purge infectious diseases from the body. The health of your immune system is mostly determined by lifestyle choices and your environment, not your genetics.
4 Ways to Boost Your Immune System
So, if your immune system health is mostly under your control, what are the most effective ways to improve your immune function?
They are, in this order:
- Exercise at least 30 minutes per day (more is better!).
- Sleep at least 7 to 9 hours per night.
- Manage your stress levels.
- Limit your alcohol intake.
Exercise At Least 30 Minutes Every Day (More Is Better!)
You probably already know that exercise reduces your risk of a long list of non-contagious diseases like heart disease, cancer, and diabetes, but it also significantly reduces the risk of contagious diseases caused by viruses and bacteria.
Scientists are still figuring out exactly how exercise improves immune function, but a few of the proposed mechanisms include:
- Improving the production and function of antibodies produced by white blood cells
- Killing bacteria via the brief rise in body temperature that occurs during and after exercise
- “Flushing” bacteria and viruses out of the lungs and airways
- Improving the production and activity of white blood cells
In fact, research shows that exercise alters “. . . the behavior of almost all immune cell populations in the bloodstream . . .”
One study conducted by scientists at the Lyon-Sud Hospital Center found that exercise particularly reduces the risk of upper respiratory tract infections in the elderly—which would make it seem like a perfect fit for defending against a disease like COVID-19.
At this point, there’s more or less no question in the scientific community that moderate exercise (usually defined as 30 to 40 minutes of moderate intensity activity a few times per week) improves immune function and reduces the risk of illness.
That said, you may have also heard that intense exercise can decrease immune function.
For example, a review study published by scientists at the University of Illinois in 2010 opened with this bold claim: “Prolonged, intense exercise causes immunosuppression, while moderate intensity exercise improves immune function and potentially reduces risk and severity of respiratory viral infection.”
The general idea is that immediately after a workout, your immune system actually becomes weaker for several hours before it has time to recover and grow stronger (just like your muscles do).
Some scientists even refer to this period of time after a hard workout as an “open-window” for viruses and bacteria to cause disease while your immune system is out of commission.
Is this true, though?
This idea originated when several early studies on endurance exercise (aka “cardio”) found that intense, prolonged workouts caused a drop in salivary markers of immune health, a decrease in white blood cell levels, and a higher risk of infection immediately post-exercise. Several studies in mice have also found that prolonged exercise increases the risk of infection after being exposed to influenza virus.
So, it would seem like intense exercise should increase your risk of infection, right?
Wrong.
Thanks to the work of researchers John P. Campbell and James E. Turner, we know this isn’t the case. In a paper aptly called “Debunking the Myth of Exercise-Induced Immune Suppression,” the authors shred the core tenets of the “open-window” hypothesis:
- They point out that most of the studies showing an increased risk of infection post-exercise were based on anecdotal reports, and many of the athletes who supposedly had upper respiratory tract infections really had other issues like asthma or lung inflammation from breathing in lots of cold air during their workouts. For example, in one study where 37 athletes claimed they had an infection, lab tests proved only 11 of them (30%) were really sick.
- Although some studies have shown that the fittest and fastest athletes have a slightly higher risk of infection, it’s highly unlikely this is due to getting sick right after their workouts, and more likely has to do with other factors such as anxiety, nutritional deficiencies, overtraining, undereating, being in close proximity to other athletes at races and workouts, frequent and prolonged travel, etc.
- Most studies show that Olympic athletes get sick about as often as the average population (and that’s despite frequent travel, high training volumes, very low body fat levels, and other factors that should increase their risk of infection).
- Most of the studies showing a significant decline in immune function and a higher risk of infection were in marathon and ultramarathon runners. It’s highly unlikely that going out for a brisk 30 to 60-minute run (often considered “intense” exercise by many) would cause similar effects, and very little data shows that other kinds of exercise (like cycling, weightlifting, swimming, etc.) cause the same negative effects.
- Most importantly, many other studies have shown that intense, prolonged exercise is associated with a lower risk of infection and better immune function. One study on elite endurance athletes found that the athletes who trained the most had the lowest incidence of infection. Two studies on ultramarathon runners found similar results. On average the runners missed only 1.5 to 2.8 days of work per year to illness, whereas average non-athletes generally miss around 4.4 days per year due to illness.
Campbell and Turner also point out that the measurement techniques often used in these studies can easily result in a “false positive” for compromised immune function in athletes, and more advanced testing shows there’s likely no significant decline in immune health after exercise.
Consistent exercise over years and decades also seems to prevent the natural decline in immune health that occurs as we age, making it particularly important for the elderly.
In the final analysis, most evidence shows that regular exercise—even intense or prolonged exercise—is good for your immune system.
So, if you already exercise regularly, keep it up, and don’t worry if you’re training “too hard” or “too much” to compromise your immune health. You probably aren’t.
And if you aren’t currently exercising, start now!
Check out these articles if you want to learn how to put together a workout routine:
The Definitive Guide on How to Build a Workout Routine
The 12 Best Science-Based Strength Training Programs for Gaining Muscle and Strength
How to Find the Best Workout Split for You
Summary: If you want to support your immune system as much as possible, keep exercising regularly (or start now if you aren’t currently). Every little bit helps, from a few light jogs per week to heavy weightlifting to training for a marathon.
Sleep At Least 7 to 9 Hours Per Night

Sleep deprivation causes a long list of problems, including muscle loss and fat gain, decreased mental function and productivity, and even makes you less attractive (seriously).
Unsurprisingly, sleep deprivation can also decrease immune health.
Researchers from the University of Washington demonstrated this in a cleverly designed study on eleven pairs of identical twins. Why use identical twins?
Well, the “optimal” sleep duration for each person is largely determined by their genetics, so by using identical twins, the researchers prevented this variable from affecting the results.
That is, each pair of twins should need about the same amount of sleep per night to maintain a healthy immune system, so any differences in their immune function should mostly be due to their sleep habits.
The researchers measured everyone’s sleep duration over a period of 14 days, and analyzed blood samples on the 15th day of the study, looking at genetic changes associated with immune function.
They found that twins who slept less than their siblings each night experienced genetic changes that are highly correlated with worse immune function over the long-term.
One problem with this study is that it only looked at genetic markers of immune function, not the actual likelihood of someone getting sick. Luckily, scientists at the University of California conducted just such a study that looked at the link between sleep deprivation and your risk of getting sick after being exposed to a disease.
In this case, scientists had 164 healthy men and women aged 18 to 55 monitor and record their sleep habits for seven days. Then, everyone was given nasal drops containing rhinovirus (the family of viruses that cause the common cold) and quarantined and monitored for 5 days.
The participants were said to have a cold when lab tests were positive and they had obvious symptoms (such as a runny nose, cough, etc.).
The researchers found that those who slept less than 5 hours per night were at the highest risk of developing a cold, people who slept 5 to 6 hours per night were at a higher risk than those who slept 7 hours per night, but those who slept 6 to 7 hours per night were at no higher risk than those who slept more than 7 hours per night.
Here’s the main takeaway from the study: people who slept less than 6 hours per night were 4.2 times more likely to catch a cold than those who slept more than 7 hours per night.
Here’s what the results looked like:
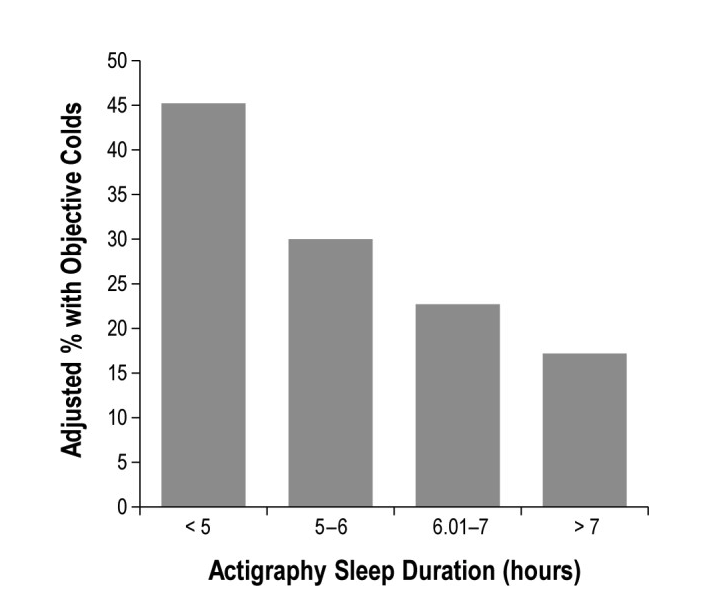
As you can see, the people who slept the least had the highest risk of getting a cold, and the people who slept the most had the lowest risk of getting a cold.
It’s worth noting that according to the CDC, most people should get around 7 to 9 hours of sleep per night for optimal health. Although the people who slept 6 to 7 hours per night weren’t at a statistically higher risk of getting a cold in this study than the people sleeping 7+ hours per night, it’s important to remember that this study only lasted a few days. It’s entirely possible that if the 6-to-7-hour-per night people maintained this schedule for weeks, months, or years, they’d wind up getting sick more often than if they slept longer.
To be fair, though, there are people who don’t need as much sleep as the average person to maintain optimal health, and who might be able to get by on 6, 5, or even 4 hours of sleep per night.
That said, the number of people who think they’re one of these outliers is a lot smaller than the number of actual outliers.
You can find out if you’re one of these people who can get by with very little sleep with the following protocol:
- Sleep in a quiet, completely dark, cool room
- Don’t set an alarm
- Go to bed at the same time every night
- Avoid all stimulants and stressful stimuli
Then, let yourself sleep as much as you need every night. Track how long you sleep each night and, after several weeks, average the numbers. The result is probably how much sleep you should aim for each night (and chances are good it’s around 7 to 9 hours).
Summary: Sleep deprivation significantly decreases immune function and increases the risk of infection, and one of the best ways to ensure your immune system is operating at peak capacity is to get as much sleep as your body needs every night (7 to 9 hours for most people).
Manage Your Stress Levels

Scientists have long suspected that stress can suppress the immune system, but thanks to several new studies published in the past decade, we now know this is the case.
For example, in one study conducted by scientists at Carnegie Mellon University, the researchers exposed 276 healthy adults to one of two kinds of rhinoviruses, and then quarantined and monitored them for five days.
The researchers asked the participants about their stress levels and measured their age, body mass index (BMI), race, sex, education status, and a variety of other factors. Finally, they also tested the participants’ level of glucocorticoid receptor resistance (GCR), a marker of compromised immune function.
Generally, the immune systems of people with GCR have trouble mounting an appropriate response to infections, often overreacting and making the symptoms of the illness worse. (This is one of the ways COVID-19 kills—by causing the immune system to overreact in a “cytokine storm” that causes organ failure and death).
The researchers found that people who had recently been through a “long-term threatening stressful experience” had the highest levels of GCR and were the most likely to develop a cold after being exposed to rhinovirus.
Another oft-cited study conducted by scientists at Ohio State University found that first year medical students’ levels of natural killer cells plummeted during exams—when they were most stressed.
Although there’s still a lot we don’t know about the link between stress and immune function, it’s clear that prolonged, intense stress seems to decrease it.
Here are a few ways to help keep your stress levels in check:
- Keep problems in perspective. Is having slow wifi for a few minutes really worth fretting about? Is it really that big of a deal if the grocery store doesn’t have your favorite brand of Greek yogurt? Is spending an extra ten or twenty minutes stuck in traffic, listening to a podcast or audiobook, really worth losing your cool over? Probably not . . .
- Prioritize the big things, pigeonhole the little things. If you’re like most people, you feel like you have a million “critical” problems that need to get done ASAP. In reality, though, you probably have one or two things that really need to get done quickly, and the rest can wait until those are finished. Often, one of the main sources of stress is simply the inability to decide what’s important and what isn’t. Get the important stuff done first, ignore everything else, and then come back to it once you’ve knocked the big items off your list.
- Hope for the best, plan for the worst. Thomas Jefferson once wrote to James Madison, “There are, indeed . . . gloomy and hypochondriac minds. . . always counting that the worst will happen, because it may happen. To these I say, how much pain have cost us the evils which have never happened!”
Psychologists refer to this as catastrophizing—convincing oneself a situation is far worse than it really is, often before it’s even happened. Coronavirus is spreading around the globe, the economy is tanking, the media won’t stop talking about climate change, the chemicals in your carpet are secretly poisoning you, etc., etc., ad infinitum. The fact is there will always be big, “scary” things happening in the world that feel out of your control, but in most cases they end up fizzling out in a few months.
Be prepared and proactive, yes, but as Jefferson wisely cautioned, hope for the best, face reality as it is, and don’t blow events out of proportion. Chances are good it’ll work out in the end, and in the case of coronavirus, stressing out about the situation may actually increase your risk of getting the disease.
Summary: Chronically high stress levels compromise immune function and increase your risk of infection. Use the strategies outlined above to manage your stress levels and keep your immune system humming along.
Limit Your Alcohol Intake

Scientists have known for decades that heavy drinking is linked with worse immune function, a higher risk of infectious diseases such as pneumonia, tuberculosis, and acute respiratory distress syndrome.
For example, a study conducted by scientists at Aarhus University Hospital found that people who drank heavily multiple times per week (>7 drinks per week) had a higher risk of being hospitalized with pneumonia than those who drank 0 to 6 times per week.
While more or less all scientists agree that binge drinking and alcoholism can impair immune function, it’s not as clear what effect moderate drinking has on your immune system.
A review study conducted by researchers at the Spanish National Research Council found that moderate drinking (10 to 14 grams of alcohol per day or less for women and 20 to 24 or less for men) was associated with slightly better immune function than abstinence. That said, other controlled trials have found that moderate drinking isn’t likely to help or hurt immune function.
The takeaway?
If you already drink moderately, giving up alcohol entirely is unlikely to reduce your risk of getting sick. That said, if you have a tendency to flirt with the line between “moderate” and “excessive” drinking, it’s a good time to cut back and play it safe.
And if you don’t currently drink, there’s no reason to start now.
If you want to learn more about the health effects of alcohol and what constitutes “light,” “moderate,” and “excessive” drinking, read this article:
How Bad Is Alcohol for You, Really?
Summary: Binge drinking and alcoholism can significantly impair immune function and increase the risk of many infectious diseases (particularly respiratory diseases like COVID-19), but moderate drinking likely has no effect on immune function.
The Bottom Line on Boosting Your Immune System
The immune system is an incredibly complex, sophisticated, and effective network of cells, tissues, and organs that protects your body from viruses, bacteria, and other pathogens 24/7, 365 days per year.
Research shows only a small fraction of our immune function is dictated by our genetics, and that about 75% of our immune health is under our control.
What, specifically can you control to ensure your immune system is in top-top shape?
Here are the biggies you need to get right:
- Exercise at least 30 minutes every day (with more being better).
- Sleep at least 7 to 9 hours per night.
- Manage your stress levels
- Limit your alcohol intake
Do that, and continue with preventative measures like washing your hands frequently, avoiding large groups of people, and trying not to touch your face, mouth, or eyes, and your risk of getting infected will be considerably lower than the average person.
What do you think of these strategies for boosting the immune system? Anything else you’d like to share? Let me know in the comments section below!
Scientific References +
- Holick MF, Binkley NC, Bischoff-Ferrari HA, et al. Evaluation, treatment, and prevention of vitamin D deficiency: An endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2011;96(7):1911-1930. doi:10.1210/jc.2011-0385
- Martineau AR, Jolliffe DA, Hooper RL, et al. Vitamin D supplementation to prevent acute respiratory tract infections: Systematic review and meta-analysis of individual participant data. BMJ. 2017;356. doi:10.1136/bmj.i6583
- Ginde AA, Blatchford P, Breese K, et al. High-Dose Monthly Vitamin D for Prevention of Acute Respiratory Infection in Older Long-Term Care Residents: A Randomized Clinical Trial. J Am Geriatr Soc. 2017;65(3):496-503. doi:10.1111/jgs.14679
- Bouillon R, Carmeliet G, Verlinden L, et al. Vitamin D and human health: Lessons from vitamin D receptor null mice. Endocr Rev. 2008;29(6):726-776. doi:10.1210/er.2008-0004
- Bikle DD. Vitamin D and bone. Curr Osteoporos Rep. 2012;10(2):151-159. doi:10.1007/s11914-012-0098-z
- Annweiler C, Rolland Y, Schott AM, Blain H, Vellas B, Beauchet O. Serum vitamin D deficiency as a predictor of incident non-Alzheimer dementias: A 7-year longitudinal study. Dement Geriatr Cogn Disord. 2012;32(4):273-278. doi:10.1159/000334944
- Huang Y, Li X, Wang M, et al. Lipoprotein lipase links vitamin D, insulin resistance, and type 2 diabetes: A cross-sectional epidemiological study. Cardiovasc Diabetol. 2013;12(1):17. doi:10.1186/1475-2840-12-17
- Pilz S, Tomaschitz A, Drechsler C, Dekker JM, März W. Vitamin D deficiency and myocardial diseases. Mol Nutr Food Res. 2010;54(8):1103-1113. doi:10.1002/mnfr.200900474
- F. Holick M. Vitamin D: Evolutionary, Physiological and Health Perspectives. Curr Drug Targets. 2010;12(1):4-18. doi:10.2174/138945011793591635
- Hemilä H, Chalker E. Vitamin C for preventing and treating the common cold. Cochrane Database Syst Rev. 2013;2013(1). doi:10.1002/14651858.CD000980.pub4
- Anderson TW, Suranyi G, Beaton GH. The effect on winter illness of large doses of vitamin C. Can Med Assoc J. 1974;111(1):31-36. https://www.ncbi.nlm.nih.gov/pubmed/4601508. Accessed March 24, 2020.
- Carr AC, Maggini S. Vitamin C and immune function. Nutrients. 2017;9(11). doi:10.3390/nu9111211
- Hemilä H. Zinc lozenges and the common cold: a meta-analysis comparing zinc acetate and zinc gluconate, and the role of zinc dosage. JRSM Open. 2017;8(5):205427041769429. doi:10.1177/2054270417694291
- Singh M. Zinc for the common cold. https://www.ncbi.nlm.nih.gov/pubmed/21328251. Accessed March 24, 2020.
- Mohsenpour B. Relation between serum zinc levels and recurrent urinary tract infections in female patients: A case-control study. - PubMed - NCBI. https://www.ncbi.nlm.nih.gov/pubmed/31456957. Accessed March 24, 2020.
- Eijkelkamp BA, Morey JR, Neville SL, et al. Dietary zinc and the control of Streptococcus pneumoniae infection. PLoS Pathog. 2019;15(8):e1007957. doi:10.1371/journal.ppat.1007957
- Niccum BA, Stein DJ, Behm BW, Hays RA. Zinc Deficiency and the Recurrence of Clostridium difficile Infection after Fecal Microbiota Transplant: A Retrospective Cohort Study. J Nutr Metab. 2018;2018:9682975. doi:10.1155/2018/9682975
- High KP, Case D, Hurd D, et al. A Randomized, Controlled Trial of Panax quinquefolius Extract (CVT-E002) to Reduce Respiratory Infection in Patients With Chronic Lymphocytic Leukemia. J Support Oncol. 2012;10(5):195-201. doi:10.1016/j.suponc.2011.10.005
- Supe A, Purandare H. Immunomodulatory role of Tinospora cordifolia as an adjuvant in surgical treatment of diabetic foot ulcers: a prospective randomized controlled study. Indian J Med Sci. 2007;61(6):347. doi:10.4103/0019-5359.32682
- McElhaney JE, Goel V, Toane B, Hooten J, Shan JJ. Efficacy of COLD-fX in the prevention of respiratory symptoms in community-dwelling adults: A randomized, double-blinded, placebo controlled trial. J Altern Complement Med. 2006;12(2):153-157. doi:10.1089/acm.2006.12.153
- McElhaney JE, Gravenstein S, Cole SK, et al. A Placebo-Controlled Trial of a Proprietary Extract of North American Ginseng (CVT-E002) to Prevent Acute Respiratory Illness in Institutionalized Older Adults. J Am Geriatr Soc. 2004;52(1):13-19. doi:10.1111/j.1532-5415.2004.52004.x
- Qi B, Wang S, Wang Q, et al. Characterization and immunostimulating effects on murine peritoneal macrophages of a novel protein isolated from Panax quinquefolius L. J Ethnopharmacol. 2016;193:700-705. doi:10.1016/j.jep.2016.10.034
- Yan J, Ma Y, Zhao F, Gu W, Jiao Y. Identification of immunomodulatory signatures induced by american ginseng in murine immune cells. Evid Based Complement Alternat Med. 2013;2013:972814. doi:10.1155/2013/972814
- Ghosh R, Smith SA, Nwangwa EE, et al. Panax quinquefolius (North American ginseng) cell suspension culture as a source of bioactive polysaccharides: Immunostimulatory activity and characterization of a neutral polysaccharide AGC1. Int J Biol Macromol. 2019;139:221-232. doi:10.1016/j.ijbiomac.2019.07.215
- Jeong YY, Park HJ, Cho YW, et al. Aged red garlic extract reduces cigarette smoke extract-induced cell death in human bronchial smooth muscle cells by increasing intracellular glutathione levels. Phyther Res. 2012;26(1):18-25. doi:10.1002/ptr.3502
- Yeh YY, Liu L. Cholesterol-lowering effect of garlic extracts and organosulfur compounds: human and animal studies. J Nutr. 2001;131(3s):989S-93S. doi:10.1093/jn/131.3.989S
- V.N. L, N. A, I. Z, et al. Beneficial effects of aged garlic extract and coenzyme Q10 on vascular elasticity and endothelial function: the FAITH randomized clinical trial. Nutrition. 2013;29(1):71-75. http://ovidsp.ovid.com/ovidweb.cgi?T=JS&CSC=Y&NEWS=N&PAGE=fulltext&D=medl&AN=22858191. Accessed March 24, 2020.
- Budoff MJ, Takasu J, Flores FR, et al. Inhibiting progression of coronary calcification using Aged Garlic Extract in patients receiving statin therapy: A preliminary study. Prev Med (Baltim). 2004;39(5):985-991. doi:10.1016/j.ypmed.2004.04.012
- Ried K, Frank OR, Stocks NP. Aged garlic extract reduces blood pressure in hypertensives: A dose-response trial. Eur J Clin Nutr. 2013;67(1):64-70. doi:10.1038/ejcn.2012.178
- Josling P. Preventing the common cold with a garlic supplement: a double-blind, placebo-controlled survey. Adv Ther. 18(4):189-193. doi:10.1007/bf02850113
- Nantz MP, Rowe CA, Muller CE, Creasy RA, Stanilka JM, Percival SS. Supplementation with aged garlic extract improves both NK and γδ-T cell function and reduces the severity of cold and flu symptoms: A randomized, double-blind, placebo-controlled nutrition intervention. Clin Nutr. 2012;31(3):337-344. doi:10.1016/j.clnu.2011.11.019
- Richard S. Rivlin. Historical Perspective on the Use of Garlic. J Nutr. 2001;131(2):604S-615S. doi:10.1093/JN
- Badar VA, Thawani VR, Wakode PT, et al. Efficacy of Tinospora cordifolia in allergic rhinitis. J Ethnopharmacol. 2005;96(3):445-449. doi:10.1016/j.jep.2004.09.034
- Lizogub VG, Riley DS, Heger M. Efficacy of a Pelargonium Sidoides Preparation in Patients With the Common Cold: A Randomized, Double Blind, Placebo-Controlled Clinical Trial. Explor J Sci Heal. 2007;3(6):573-584. doi:10.1016/j.explore.2007.09.004
- Agbabiaka TB, Guo R, Ernst E. Pelargonium sidoides for acute bronchitis: A systematic review and meta-analysis. Phytomedicine. 2008;15(5):378-385. doi:10.1016/j.phymed.2007.11.023
- Janecki A, Conrad A, Engels I, Frank U, Kolodziej H. Evaluation of an aqueous-ethanolic extract from Pelargonium sidoides (EPs® 7630) for its activity against group A-streptococci adhesion to human HEp-2 epithelial cells. J Ethnopharmacol. 2011;133(1):147-152. doi:10.1016/j.jep.2010.09.018
- Watzl B, Bub A, Briviba K, Rechkemmer G. Acute intake of moderate amounts of red wine or alcohol has no effect on the immune system of healthy men. Eur J Nutr. 2002;41(6):264-270. doi:10.1007/s00394-002-0384-0
- Watzl B, Bub A, Pretzer G, Roser S, Barth SW, Rechkemmer G. Daily moderate amounts of red wine or alcohol have no effect on the immune system of healthy men. Eur J Clin Nutr. 2004;58(1):40-45. doi:10.1038/sj.ejcn.1601742
- Díaz LE, Montero A, González-Gross M, Vallejo AI, Romeo J, Marcos A. Influence of alcohol consumption on immunological status: A review. Eur J Clin Nutr. 2002;56:S50-S53. doi:10.1038/sj.ejcn.1601486
- Kornum JB, Due KM, Nørgaard M, et al. Alcohol drinking and risk of subsequent hospitalisation with pneumonia. Eur Respir J. 2012;39(1):149-155. doi:10.1183/09031936.00000611
- Cohen S, Janicki-Deverts D, Doyle WJ, et al. Alcohol and the Immune System. Proc Natl Acad Sci U S A. 2012;109(16):5995-5999. doi:10.1073/pnas.1118355109
- Kiecolt-Glaser JK, Garner W, Speicher C, Penn GM, Holliday J, Glaser R. Psychosocial modifiers of immunocompetence in medical students. Psychosom Med. 1984;46(1):7-14. doi:10.1097/00006842-198401000-00003
- Mehta P, Mcauley DF, Brown M, et al. Correspondence COVID-19 : consider cytokine storm syndromes and. Lancet. 2020;6736(20):19-20. doi:10.1016/S0140-6736(20)30628-0
- Cohen S, Janicki-Deverts D, Doyle WJ, et al. Chronic stress, glucocorticoid receptor resistance, inflammation, and disease risk. Proc Natl Acad Sci U S A. 2012;109(16):5995-5999. doi:10.1073/pnas.1118355109
- Sehgal A, Mignot E. Genetics of sleep and sleep disorders. Cell. 2011;146(2):194-207. doi:10.1016/j.cell.2011.07.004
- Prather AA, Janicki-Deverts D, Hall MH, Cohen S. Behaviorally Assessed Sleep and Susceptibility to the Common Cold. Sleep. 2015;38(9):1353-1359. doi:10.5665/sleep.4968
- Ambrosius U, Lietzenmaier S, Wehrle R, et al. Heritability of Sleep Electroencephalogram. Biol Psychiatry. 2008;64(4):344-348. doi:10.1016/j.biopsych.2008.03.002
- De Gennaro L, Marzano C, Fratello F, et al. The electroencephalographic fingerprint of sleep is genetically determined: A twin study. Ann Neurol. 2008;64(4):455-460. doi:10.1002/ana.21434
- Killgore WDS. Transcriptional Signatures of Sleep Duration Discordance in Monozygotic Twins. In: Progress in Brain Research. Vol 185. Elsevier B.V.; 2010:105-129. doi:10.1016/B978-0-444-53702-7.00007-5
- Sundelin T, Lekander M, Sorjonen K, Axelsson J. Negative effects of restricted sleep on facial appearance and social appeal. R Soc Open Sci. 2017;4(5). doi:10.1098/rsos.160918
- Magnavita N, Garbarino S. Sleep, health and wellness at work: A scoping review. Int J Environ Res Public Health. 2017;14(11). doi:10.3390/ijerph14111347
- Killgore WDS. Effects of sleep deprivation on cognition. In: Progress in Brain Research. Vol 185. Elsevier B.V.; 2010:105-129. doi:10.1016/B978-0-444-53702-7.00007-5
- Nedeltcheva A V., Kilkus JM, Imperial J, Schoeller DA, Penev PD. Insufficient sleep undermines dietary efforts to reduce adiposity. Ann Intern Med. 2010;153(7):435. doi:10.1059/0003-4819-153-7-201010050-00006
- Nieman DC, Wentz LM. The compelling link between physical activity and the body’s defense system. J Sport Heal Sci. 2019;8(3):201-217. doi:10.1016/j.jshs.2018.09.009
- Hoffman MD, Fogard K. Demographic characteristics of 161-km ultramarathon runners. Res Sport Med. 2012;20(1):59-69. doi:10.1080/15438627.2012.634707
- Hoffman MD, Krishnan E. Health and exercise-related medical issues among 1,212 ultramarathon runners: Baseline findings from the Ultrarunners Longitudinal TRAcking (ULTRA) Study. PLoS One. 2014;9(1):e83867. doi:10.1371/journal.pone.0083867
- Mårtensson S, Nordebo K, Malm C. High training volumes are associated with a low number of self-reported sick days in elite endurance athletes. J Sport Sci Med. 2014;13(4):929-933. https://www.ncbi.nlm.nih.gov/pubmed/25435787/. Accessed March 24, 2020.
- Fondell E, Lagerros YT, Sundberg CJ, et al. Physical activity, stress, and self-reported upper respiratory tract infection. Med Sci Sports Exerc. 2011;43(2):272-279. doi:10.1249/MSS.0b013e3181edf108
- Bonini M, Gramiccioni C, Fioretti D, et al. Asthma, allergy and the olympics: A 12-year survey in elite athletes. Curr Opin Allergy Clin Immunol. 2015;15(2):184-192. doi:10.1097/ACI.0000000000000149
- Derman W, Schwellnus M, Jordaan E. Clinical characteristics of 385 illnesses of athletes with impairment reported on the web-iiss system during the london 2012 paralympic games. PM R. 2014;6(8 SUPPL.):S23-30. doi:10.1016/j.pmrj.2014.05.016
- Campbell JP, Turner JE. Debunking the myth of exercise-induced immune suppression: Redefining the impact of exercise on immunological health across the lifespan. Front Immunol. 2018;9(APR). doi:10.3389/fimmu.2018.00648
- Spence L, Brown WJ, Pyne DB, et al. Incidence, etiology, and symptomatology of upper respiratory illness in elite athletes. Med Sci Sports Exerc. 2007;39(4):577-586. doi:10.1249/mss.0b013e31802e851a
- Campbell JP, Turner JE. Debunking the myth of exercise-induced immune suppression: Redefining the impact of exercise on immunological health across the lifespan. Front Immunol. 2018;9(APR). doi:10.3389/fimmu.2018.00648
- Murphy EA, Davis JM, Carmichael MD, Gangemi JD, Ghaffar A, Mayer EP. Exercise stress increases susceptibility to influenza infection. Brain Behav Immun. 2008;22(8):1152-1155. doi:10.1016/j.bbi.2008.06.004
- Heath GW, Ford ES, Craven TE, Macera CA, Jackson KL, Pate RR. Exercise and the incidence of upper respiratory tract infections. Med Sci Sports Exerc. 1991;23(2):152-157. doi:10.1249/00005768-199102000-00002
- Nieman DC, Henson DA, Fagoaga OR, et al. Change in salivary IgA following a competitive marathon race. Int J Sports Med. 2002;23(1):69-75. doi:10.1055/s-2002-19375
- Mackinnon LT, Ginn E, Seymour GJ. Decreased salivary immunoglobulin A secretion rate after intense interval exercise in elite kayakers. Eur J Appl Physiol Occup Physiol. 1993;67(2):180-184. doi:10.1007/bf00376664
- Kakanis MW, Peake J, Brenu EW, et al. The open window of susceptibility to infection after acute exercise in healthy young male elite athletes. Exerc Immunol Rev. 2010;16:119-137. doi:10.1016/j.jsams.2010.10.642
- Kostka T, Berthouze SE, Lacour JR, Bonnefoy M. The symptomatology of upper respiratory tract infections and exercise in elderly people. Med Sci Sports Exerc. 2000;32(1):46-51. doi:10.1097/00005768-200001000-00008
- Walsh NP, Gleeson M, Shephard RJ, et al. Position statement part one: Immune function and exercise. Exerc Immunol Rev. 2011;17:6-63. https://www.ncbi.nlm.nih.gov/pubmed/21446352. Accessed March 24, 2020.
- Walsh NP, Gleeson M, Pyne DB, et al. Position statement part two: Maintaining immune health. Exerc Immunol Rev. 2011;17:64-103. https://www.ncbi.nlm.nih.gov/pubmed/21446353. Accessed March 24, 2020.
- Baik I, Curhan GC, Rimm EB, Bendich A, Willett WC, Fawzi WW. A prospective study of age and lifestyle factors in relation to community-acquired pneumonia in US men and women. Arch Intern Med. 2000;160(20):3082-3088. doi:10.1001/archinte.160.20.3082
- Romaniszyn D, Pobiega M, Wójkowska-Mach J, et al. The general status of patients and limited physical activity as risk factors of Methicillin-resistant Staphylococcus aureus occurrence in long-term care facilities residents in Krakow, Poland. BMC Infect Dis. 2014;14(1):271. doi:10.1186/1471-2334-14-271
- Leveille SG, Gray S, Lacroix AZ, Ferrucci L, Black DJ, Guralnik JM. Physical inactivity and smoking increase risk for serious infections in older women. J Am Geriatr Soc. 2000;48(12):1582-1588. doi:10.1111/j.1532-5415.2000.tb03867.x
- Pape K, Ryttergaard L, Rotevatn TA, et al. Leisure-Time Physical Activity and the Risk of Suspected Bacterial Infections. Med Sci Sports Exerc. 2016;48(9):1737-1744. doi:10.1249/MSS.0000000000000953
- Warburton DER, Bredin SSD. Health benefits of physical activity: A systematic review of current systematic reviews. Curr Opin Cardiol. 2017;32(5):541-556. doi:10.1097/HCO.0000000000000437
- Brodin P, Jojic V, Gao T, et al. Variation in the human immune system is largely driven by non-heritable influences. Cell. 2015;160(1-2):37-47. doi:10.1016/j.cell.2014.12.020
- Mikkola J, Rusko H, Izquierdo M, Gorostiaga EM, Häkkinen K. Neuromuscular and cardiovascular adaptations during concurrent strength and endurance training in untrained men. Int J Sports Med. 2012;33(9):702-710. doi:10.1055/s-0031-1295475
- Riou J, Hauser A, Counotte MJ, Althaus CL. Adjusted age-specific case fatality ratio during the COVID-19 epidemic in Hubei, China, January and February 2020. medRxiv. March 2020:2020.03.04.20031104. doi:10.1101/2020.03.04.20031104
- Paget J, Spreeuwenberg P, Charu V, et al. Global mortality associated with seasonal influenza epidemics: New burden estimates and predictors from the GLaMOR Project. J Glob Health. 2019;9(2). doi:10.7189/jogh.09.020421
- Estimating the infection and case fatality ratio for COVID-19 using age-adjusted data from the outbreak on the Diamond Princess cruise ship | CMMID Repository. https://cmmid.github.io/topics/covid19/severity/diamond_cruise_cfr_estimates.html. Accessed March 24, 2020.
- Wu JT, Leung K, Bushman M, et al. Estimating clinical severity of COVID-19 from the transmission dynamics in Wuhan, China. Nat Med. March 2020:1-5. doi:10.1038/s41591-020-0822-7










