High blood pressure is a condition that affects around 3.5 billion people worldwide.
Despite its prevalence, many people have a limited understanding of its symptoms, causes, and consequences.
In this article, we’ll unravel the complexities of high blood pressure to help you navigate the confusing terrain of hypertension with greater confidence.
You’ll also learn science-backed strategies to help you lower your blood pressure, which may help you live a healthier, longer life.
What Is Blood Pressure?
Blood pressure is the force exerted by circulating blood on the walls of blood vessels. It’s one of the primary parameters health professionals use to assess the health of your cardiovascular system.
Blood pressure has two key measurements: systolic and diastolic.
Systolic blood pressure measures the pressure in the arteries when the heart contracts (pumps blood), while diastolic blood pressure measures the pressure when the heart rests between beats.
When we write these numbers, we separate them with a forward slash (/), with the systolic reading to the left and the diastolic reading to the right.
How Do You Measure Blood Pressure?
Traditionally, healthcare professionals use a sphygmomanometer to measure blood pressure.
This manual device includes an inflatable blood pressure cuff that wraps around your arm and a meter to record the pressure.
The clinician inflates the cuff, constricting your artery and obstructing the blood flow. As the cuff deflates, they use a stethoscope to listen for the return and steady flow of blood.
These points mark the systolic and diastolic pressures, respectively.
In contrast, digital blood pressure monitors use electronic sensors to detect blood flow. After you secure the cuff around your arm and the cuff inflates, the monitor measures the pressure at which blood starts to flow (systolic pressure) and the pressure when the heart rests between beats (diastolic pressure). The monitor then displays these readings digitally.
Using an electronic blood pressure monitor simplifies the measuring process, hence their popularity in most healthcare and home settings.
Whether you’re using a sphygmomanometer or a digital blood pressure monitor, it’s essential to sit quietly for a few minutes before taking the measurement and to position your arm at heart level to ensure the most accurate results.
What Is Normal Blood Pressure?
According to the American Heart Association, normal blood pressure in people not taking antihypertensive (blood-pressure lowering) medication is approximately 120/80 mmHg.
However, normal blood pressure can vary from person to person and can change based on factors such as stress, sleep, and physical activity.
What Is High Blood Pressure?
High blood pressure, or hypertension, occurs when your blood pressure consistently measures at 130/80 mm Hg or above.
Hypertension is a significant health concern because it puts additional strain on your heart and blood vessels, thereby elevating your risk of heart disease, heart failure, and stroke.
What Are the Symptoms of High Blood Pressure?
High blood pressure often presents no obvious symptoms, earning it the moniker “the silent killer.”
However, in extreme cases, high blood pressure symptoms may include headaches, shortness of breath, dizziness, chest pain, heart palpitations, and low mood.
What Causes High Blood Pressure?
Several factors contribute to the development of high blood pressure, including age, genetic predisposition, body weight, and lifestyle habits, as well as certain medical conditions.
- Age: Blood vessels naturally stiffen and lose flexibility as we age, increasing blood pressure. Studies show that aging is a significant risk factor for high blood pressure, with most adults experiencing rising blood pressure starting from their mid-50s.
- Family History: Research indicates that if high blood pressure is common among your close blood relatives, your risk of developing the condition increases.
- Weight: Being overweight or obese significantly increases blood pressure. According to some research, excess body fat accounts for 65-to-75% of the risk of hypertension.
- Lifestyle Habits: Habits such as excessive sodium intake, physical inactivity, heavy alcohol consumption, and tobacco use can raise your blood pressure risk. These lifestyle factors can lead to weight gain and directly impact heart and blood vessel health.
Certain underlying health conditions and medications can also lead to high blood pressure:
- Kidney Disease: Kidney disease can disrupt the kidneys’ role in regulating blood pressure, leading to fluid retention and increased blood pressure.
- Hormonal Disorders: Certain hormonal disorders, like Cushing’s syndrome, can cause high blood pressure by overproducing the stress hormone cortisol.
- Certain Medications: Some medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs), certain birth control pills, and decongestants, can raise blood pressure.
How to Lower Blood Pressure
Addressing high blood pressure requires a multi-faceted approach, incorporating diet, exercise, weight management, consuming alcohol in moderation, stress management, and, in some cases, medication.
- Diet: Adopt a diet rich in foods that lower blood pressure, including fruits, vegetables, whole grains, lean proteins, and healthy fats. If you’d like specific advice about what diet to follow to reach your health and fitness goals, take the Legion Diet Quiz, and in less than a minute, you’ll know exactly what diet is right for you.
- Exercise: Engage in at least 150 minutes of moderate-intensity or 75 minutes of high-intensity exercise each week. Some good types of exercise for lowering blood pressure include brisk walking, swimming, cycling, and strength training. If you’d like an exercise program designed to help you get fitter and healthier than ever, check out my fitness books for men and women, Bigger Leaner Stronger and Thinner Leaner Stronger .
- Weight Management: Maintain a healthy weight for your height and body composition. To achieve this, aim for a Body Mass Index (BMI) between 18.5 and 24.9.
- Alcohol: Limit alcohol consumption to moderate levels—up to one drink a day for women and up to two drinks a day for men.
- Stress Management: Incorporating stress management strategies, such as mindfulness, yoga, or deep-breathing exercises may help lower blood pressure over time.
- Medication: Sometimes, lifestyle modifications may not suffice to manage high blood pressure. If that’s true for you, your healthcare provider may prescribe blood pressure medication. Several classes of blood pressure medications exist, including diuretics, ACE inhibitors, and calcium channel blockers.
FAQ #1: What are the most important foods to avoid with high blood pressure?
Avoid foods high in sodium, such as processed meats and cheeses, canned soups and vegetables, pre-prepared meals, sauces, and salad dressings, and fast food.
You may also benefit from limiting your intake of foods high in saturated and trans fats, like fried foods, which may negatively impact blood pressure.
FAQ #2: When is blood pressure high enough to go to the hospital?
A blood pressure reading higher than 180/120 mmHg, known as hypertensive crisis, requires immediate medical attention. This condition can lead to a stroke, heart attack, or other serious health problems if not treated promptly.
FAQ #3: Can dehydration cause high blood pressure?
Dehydration may indirectly lead to high blood pressure.
In a study published in the journal Nutrients, researchers found that frequent dehydration causes changes in blood vessel function and blood pressure regulation, which may increase your risk of experiencing numerous cardiovascular issues, including high blood pressure.
FAQ #4: What is a blood pressure chart?
A blood pressure chart is a tool that categorizes blood pressure readings into different stages, from normal to high. Healthcare professionals use them to diagnose and manage blood pressure.
Here’s an example blood pressure chart:
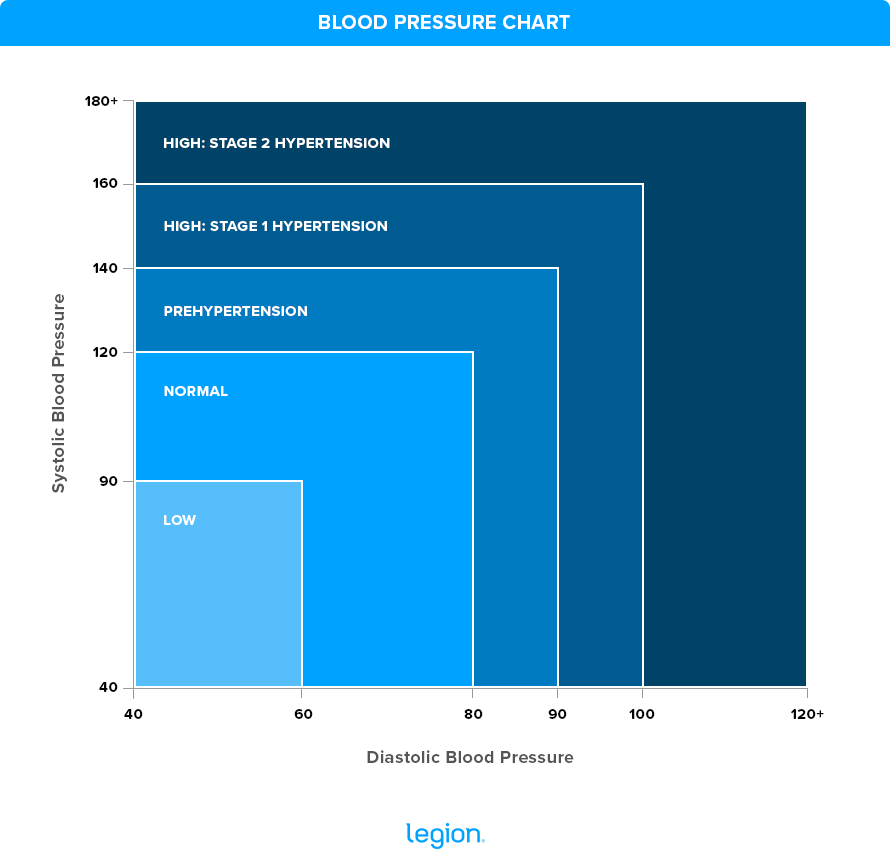
FAQ #5: What is considered a normal blood pressure range?
A normal blood pressure ranges from 90/60 mmHg up to 120/80mmHg.
However, “normal” can vary depending on a person’s health status and age. Regular monitoring is important to understand what’s normal for you and to detect any changes early.
Scientific References +
- Mills KT, Stefanescu A, He J. The global epidemiology of hypertension. Nature Reviews Nephrology. 2020;16(4):223-237. doi:https://doi.org/10.1038/s41581-019-0244-2
- Oparil S, Acelajado MC, Bakris GL, et al. Hypertension. Nature Reviews Disease Primers. 2018;4(4):1-48. doi:https://doi.org/10.1038/nrdp.2018.14
- Goodhart AK. Hypertension from the patient’s perspective. The British Journal of General Practice. 2016;66(652):570. doi:https://doi.org/10.3399/bjgp16X687757
- Franklin SS, Gustin W, Wong ND, et al. Hemodynamic Patterns of Age-Related Changes in Blood Pressure. Circulation. 1997;96(1):308-315. doi:https://doi.org/10.1161/01.cir.96.1.308
- Ehret GB. Genome-Wide Association Studies: Contribution of Genomics to Understanding Blood Pressure and Essential Hypertension. Current hypertension reports. 2010;12(1):17-25. doi:https://doi.org/10.1007/s11906-009-0086-6
- Hall JE, do Carmo JM, da Silva AA, Wang Z, Hall ME. Obesity, kidney dysfunction and hypertension: mechanistic links. Nature Reviews Nephrology. 2019;15(6):367-385. doi:https://doi.org/10.1038/s41581-019-0145-4
- Hall JE, do Carmo JM, da Silva AA, Wang Z, Hall ME. Obesity-Induced Hypertension. Circulation Research. 2015;116(6):991-1006. doi:https://doi.org/10.1161/circresaha.116.305697
- Garrison RJ, Kannel WB, Stokes J, Castelli WP. Incidence and precursors of hypertension in young adults: The Framingham offspring study. Preventive Medicine. 1987;16(2):235-251. doi:https://doi.org/10.1016/0091-7435(87)90087-9
- Aronow WS. Lifestyle measures for treating hypertension. Archives of Medical Science : AMS. 2017;13(5):1241-1243. doi:https://doi.org/10.5114/aoms.2017.68650
- Tedla FM, Brar A, Browne R, Brown C. Hypertension in Chronic Kidney Disease: Navigating the Evidence. International Journal of Hypertension. 2011;2011:1-9. doi:https://doi.org/10.4061/2011/132405
- Isidori AM, Graziadio C, Paragliola RM, et al. The hypertension of Cushingʼs syndrome. Journal of Hypertension. 2015;33(1):44-60. doi:https://doi.org/10.1097/hjh.0000000000000415
- Warner TD, Mitchell JA. COX-2 selectivity alone does not define the cardiovascular risks associated with non-steroidal anti-inflammatory drugs. The Lancet. 2008;371(9608):270-273. doi:https://doi.org/10.1016/s0140-6736(08)60137-3
- Cameron NA, Blyler CA, Bello NA. Oral Contraceptive Pills and Hypertension: A Review of Current Evidence and Recommendations. Hypertension. 2023;80(5):924-935. doi:https://doi.org/10.1161/hypertensionaha.122.20018
- Aronow WS. Drug-induced causes of secondary hypertension. Annals of Translational Medicine. 2017;5(17). doi:https://doi.org/10.21037/atm.2017.06.16
- Challa HJ, Uppaluri KR. DASH Diet (Dietary Approaches to Stop Hypertension). Nih.gov. Published 2018. https://www.ncbi.nlm.nih.gov/books/NBK482514/
- Pescatello LS, MacDonald HV, Lamberti L, Johnson BT. Exercise for Hypertension: A Prescription Update Integrating Existing Recommendations with Emerging Research. Current Hypertension Reports. 2015;17(11). doi:https://doi.org/10.1007/s11906-015-0600-y
- Landi F, Calvani R, Picca A, et al. Body Mass Index Is Strongly Associated with Hypertension: Results from the Longevity Check-up 7+ Study. Nutrients. 2018;10(12):1976. doi:https://doi.org/10.3390/nu10121976
- Briasoulis A, Agarwal V, Messerli FH. Alcohol Consumption and the Risk of Hypertension in Men and Women: A Systematic Review and Meta-Analysis. The Journal of Clinical Hypertension. 2012;14(11):792-798. doi:https://doi.org/10.1111/jch.12008
- Park SH, Han KS. Blood Pressure Response to Meditation and Yoga: A Systematic Review and Meta-Analysis. The Journal of Alternative and Complementary Medicine. 2017;23(9):685-695. doi:https://doi.org/10.1089/acm.2016.0234
- Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71(6):1269-1324. doi:https://doi.org/10.1161/hyp.0000000000000066
- Wang L, Manson JE, Forman JP, Gaziano JM, Buring JE, Sesso HD. Dietary Fatty Acids and the Risk of Hypertension in Middle-Aged and Older Women. Hypertension. 2010;56(4):598-604. doi:https://doi.org/10.1161/hypertensionaha.110.154187
- Salkic S, Batic-Mujanovic O, Ljuca F, Brkic S. Clinical Presentation of Hypertensive Crises in Emergency Medical Services. Materia Socio-Medica. 2014;26(1):12-16. doi:https://doi.org/10.5455/msm.2014.26.12-16
- Watso JC, Farquhar WB. Hydration Status and Cardiovascular Function. Nutrients. 2019;11(8):1866. doi:https://doi.org/10.3390/nu11081866










